Abstract
Introduction
Together with considerable improvement in diagnostics and supportive care measures, treatment intensification has contributed to the improvement of pediatric acute myeloid leukemia (AML) survival outcomes. However, treatment-related toxicity is a consequence of intensified chemotherapy regimens, which has profound implications for both morbidity and mortality. Despite the known devastating impact of all types of toxicity on quality of life (QoL), studies presenting the different forms of non-infectious toxicity prevalent during the most recent Dutch pediatric AML protocols are lacking given that only prior protocols have been evaluated in this manner as of yet. Furthermore, the literature on non-infectious toxicity incidence in pediatric AML patients is relatively scarce. Therefore, the objectives of this study were to: 1) evaluate the cumulative incidence (C.I.) of severe, but non-lethal, non-infectious toxicity during AML treatment according to the last three consecutive protocols of the Dutch Childhood Oncology Group (DCOG), and 2) compare treatment-related toxicity frequencies between protocols.
Methods
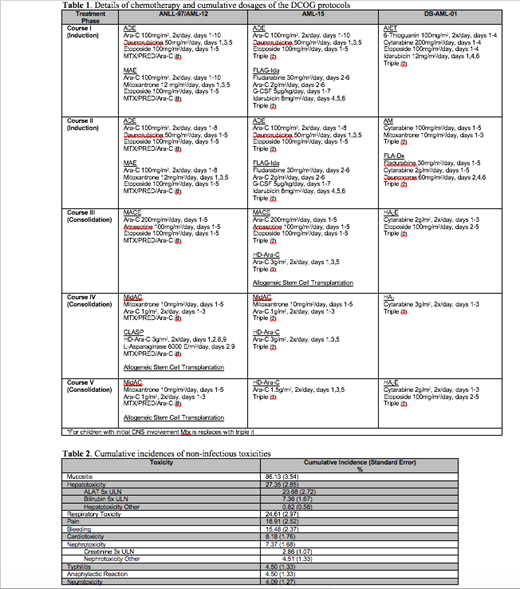
A retrospective chart review was performed on 245 Dutch patients diagnosed with de novo AML (acute promyelocytic leukemia, myeloid leukemia of Down Syndrome, and secondary AML were excluded) and treated according to ANLL-97/AML-12 (1998-2005) n=118, AML-15 (2005-2010) n=60, or DB-AML-01 (2010-2013) n=67. Table 1 details protocol specifics, including drug dosages per course. Grade 3-4 toxicities, including hematological toxicity, cardiotoxicity, respiratory toxicity, mucositis, typhlitis, nephrotoxicity, hepatotoxicity, neurotoxicity, pain, allergic anaphylactic reaction, and elevation of alanineaminotransferase or bilirubin were defined according to Common Terminology Criteria for Adverse Event version 4.0, excluding infectious toxicity. Grade 5 toxicity (treatment-related mortality) was beyond the scope of this study. Intensive care unit (ICU) admission data was additionally assessed. Toxicity C.I.s were determined via competing events analyses. Relapse and death were considered competing events. Patients were censored at time of stem cell transplantation. Per-protocol comparisons were conducted via Chi-square test, due to lack of sufficient power required to calculate C.I.s.
Results
Median age at diagnosis was 6.0 years [interquartile range (IQR) 1.0-12.0], 58% were male. Mucositis was the most frequent form of non-hematological toxicity with a C.I. of 86.1% (standard error (S.E.) 3.5%), followed by hepatotoxicity (C.I. 27.4%, S.E. 2.9%), and respiratory toxicity (C.I. 24.6%, S.E. 3.0%) (Table 2). Eighty-three patients (C.I. 33.9%, S.E. 3.0%) were admitted to the ICU at least once, for a median of 6.0 days [IQR 2.0-15.0] (Table 2).
Relatively more blood transfusions (both erythrocyte and thrombocyte) were administered to patients treated according to AML-15 (98.3%) and DB-AML-01 (97.0%) compared to AML-12 (86.4%) (p=0.01 and p=0.02, respectively). Relatively more patients suffered from severe mucositis during DB-AML-01 compared to AML-12 (43.4% vs. 25.4%, p=0.01). More patients treated according to AML-15 had bilirubin levels >3x upper limit of normal (ULN) compared to those treated according to AML-12 (13.3% vs. 3.4%, p=0.01). There were no differences in non-infectious toxicity frequency between AML-15 and DB-AML-01. Other forms of toxicity did not differ significantly between protocols. The percentage of patients admitted to the ICU at least once during treatment was 33.9% in AML-12, 26.7% in AML-15, and 40.3% in DB-AML-01.
Conclusions
The high incidence of severe short- and long-term toxicities during pediatric AML therapy poses substantial challenges for patients, families, and care providers. Mucositis was the most common form of non-hematological, non-infectious toxicity in the whole cohort and across all Dutch protocols. Toxicities were more prevalent during the more recent protocols (AML-15 and DB-AML-01) compared to AML-12. Therefore, our findings are important in that they substantiate the need to optimize pediatric AML care in a manner which decreases treatment-related toxicity and QoL impairment. High treatment-related morbidity rates stress the urge to improve supportive care and develop less toxic treatment, while maintaining efficacy.
Zwaan: Sanofi: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal